Jump to:
Planning | The Procedure | Aftercare | FAQs
Donor Harvesting Techniques: Follicular Unit Transplantation vs. Follicular Unit Excision
General Principles
Individuals have a permanent rim of hair that runs along the sides and back of the scalp. This region has less exposure to, and lower sensitivity toward, the hormones that drive hair loss. With few exceptions, the hairs in this rim are permanent and can serve as donor hairs. Hair restoration surgery is based on the principle of donor dominance—the concept that donor hairs maintain their permanent characteristics even when transplanted into balding areas. In essence, hair transplantation redistributes permanent hairs from the donor zone to areas of thinning or baldness.
Planning for the Procedure
Planning is the most important element to successful hair transplantation.
Good planning requires recognizing that hair loss is a dynamic process that typically progresses over time. Areas at risk of future thinning should be addressed during the initial procedure, or sufficient donor hair must be preserved to allow for future treatment. Likewise, the permanent donor rim gradually decreases in size and density, making it essential to harvest conservatively—avoiding overharvesting, staying clear of the rim’s periphery, and minimizing scarring.
Designs must also account for permanence. Hairlines and density patterns should suit the patient now and decades into the future; for example, a hairline placed too low in a young man may appear unnatural as he ages. Ultimately, thoughtful planning reduces long-term aesthetic risks and ensures durable, natural results that do not draw undue attention.
The Procedure
-
First:
On the morning of the procedure, the treatment plan is reviewed in detail. Patients are then given medication to help them relax, and most will sleep or drowse comfortably throughout the surgery.
-
Second:
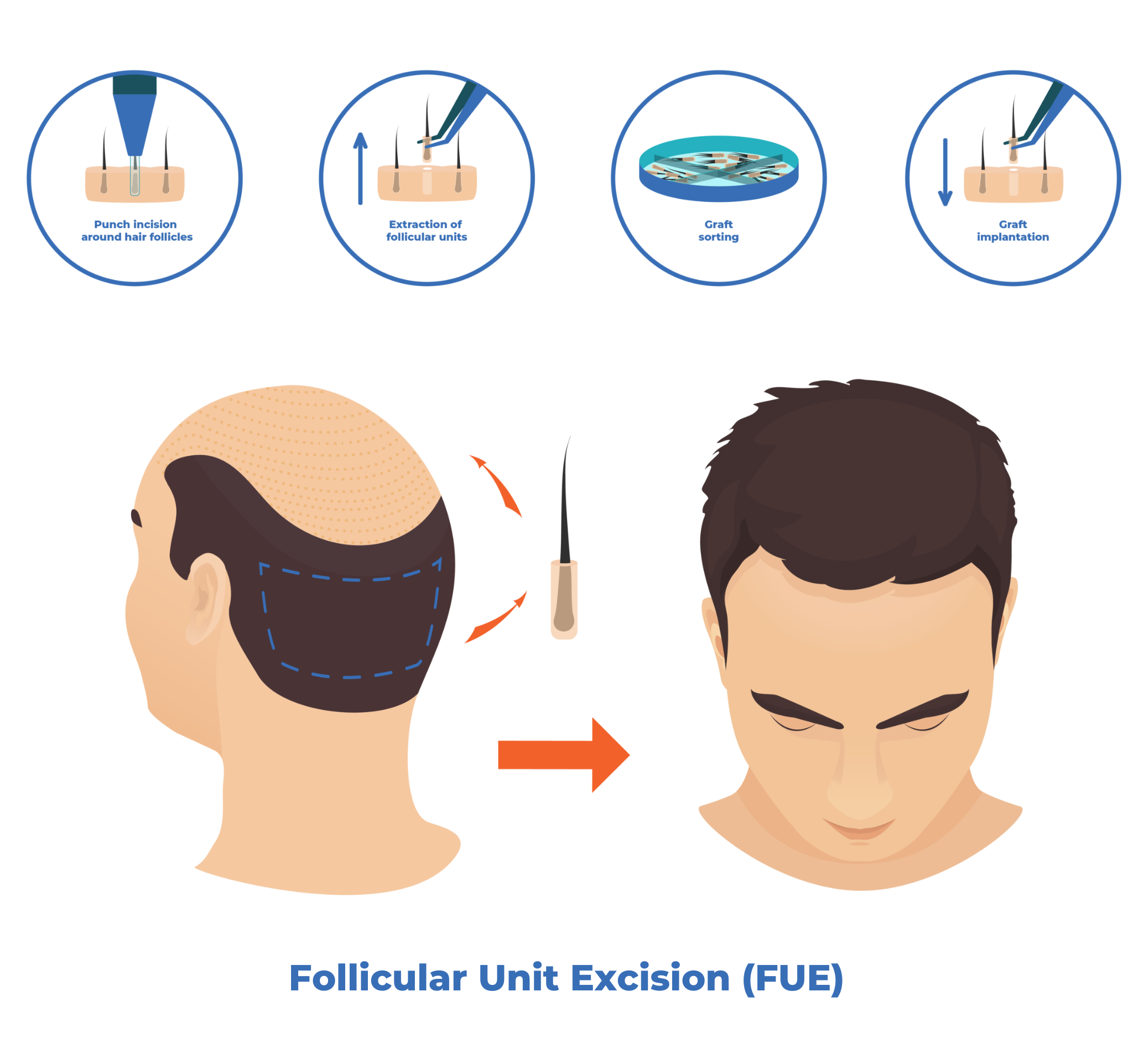
In the next step, the scalp is numbed using local anesthetic. Donor tissue is then removed using either Follicular Unit Transplanting (FUT) or Follicular Unit Excision (FUE). When FUE is performed, the scalp will typically—though not always—require shaving prior to extraction.
-
Third:
Follicular Unit Grafts (FUGs), consisting of one or several hairs, are then prepared from the harvested donor tissue. A pattern of small recipient sites is created to accommodate these grafts, each placed at the same angle and direction as existing hairs to ensure a natural appearance. This step represents the key planning and artistic component of the procedure.
-
Fourth:
After the recipient pattern has been created, the grafts are placed into these sites. The finest single-hair grafts are positioned at the periphery of the transplanted area to ensure a natural, feathered appearance, while grafts containing multiple hairs are placed more centrally to enhance density.
Aftercare (Post-op)
Initial Care
Patients return the morning after the operation for an initial follow-up visit, and again 7–10 days later for a final visit, at which time sutures are removed if FUT was used. Post-operative discomfort is minimal with both techniques.
The visibility of the procedure varies, largely based on whether the donor or recipient area was shaved. FUE requires shaving the donor area. In contrast, in FUT the donor area is not shaved and is fully camouflaged by the surrounding hair, even immediately after surgery.
The recipient area is rarely shaved, except in very large sessions. As a result, visibility depends mainly on how well the existing hair can conceal the small crusts and redness that form around grafts.
Most patients in Dr. Unger’s practice choose a no-shave FUT approach. In these cases, noticeable signs of transplantation typically resolve within a week.
Hair Growth
Short transplanted hairs are visible immediately after the operation, except in long-hair transplantation, an occasionally used technique that provides an immediate preview of the result. Transplanted hairs may grow briefly but more commonly shed two to four weeks after the procedure. New growth typically begins around four months, although these early hairs are fine and short. Noticeable cosmetic improvement is usually evident by six months, with continued maturation and additional growth over the first twelve months. Most of the final result can be assessed at approximately one year, though studies show that some growth may continue up to 15 months.
Hairlines
Follicular Unit Transplantation
Follicular Unit Transplantation (FUT) is a method of donor hair harvesting in which a single strip of tissue containing multiple follicular units is removed from the donor area. A team of experienced staff then dissects this tissue to isolate individual follicular unit grafts (FUGs). After healing, patients are typically left with a thin linear scar that is virtually undetectable unless the scalp is shaved. With subsequent procedures, the existing donor scar is removed as part of the new harvest, allowing patients to maintain a single linear scar even after multiple surgeries.
FUT offers several advantages for patients. It results in less perioperative visibility compared with follicular unit extraction, since the surrounding hair camouflages the donor area. FUT also produces less tissue trauma. For example, a 24 cm incision creates 48 cm of total incisional length, whereas extracting 2000 follicular units with a 0.9 mm punch produces approximately 565 cm of incisional length. It creates less scar tissue. A 24 cm FUT incision yields about 2.4 cm² of scar tissue, compared with approximately 12.72 cm² from 2000 FUE using a 0.9 mm punch. Graft survival is typically higher as well. Medium trimmed grafts have reported survival rates of 80 to 98 percent, whereas skeletonized grafts have survival rates of 48 to 69 percent. Finally, FUT allows donor harvesting to remain strictly within the safe donor zone, which is essential for long term natural looking results.
At the same time, FUT has meaningful disadvantages, first and foremost by restricting hairstyle flexibility to a greater degree, since patients must maintain a certain hair length to ensure camouflage of the linear donor scar.
Donor harvesting is confined to the safe donor are even as the area of balding expands
Donor Scars Post-Procedure:
Donor scar area post-procedure
Donor scar area post-procedure
Follicular Unit Excision
Follicular Unit Excision (FUE) is a donor harvesting technique in which follicular units are removed individually from the scalp in a single-step procedure. In contrast, FUT is a two-step method: a strip of tissue containing numerous follicular units is first removed, and the individual follicular units are then dissected from this tissue. After healing, FUE produces multiple small circular scars throughout the donor area, while FUT results in a single linear scar. However, unlike FUT, FUE generally allows the hair in the donor region to be clipped somewhat shorter without revealing the scar pattern.
FUE is the preferred approach for patients with less severe hair loss and who prefer shorter hairstyles, who require a smaller number of grafts, or who have insufficient scalp elasticity to safely undergo FUT. Moreover, with careful planning and patient selection, a single FUE session may provide advantages, including the possibility of temporary cosmetic benefit without committing the patient to a staged or long-term surgical plan. This can allow certain individuals who would otherwise not be ideal candidates for transplantation to receive a smaller, more tailored intervention.
However, FUE also has important disadvantages. First and foremost, in order to obtain a large number of grafts, most practitioners need to harvest grafts outside of the safe donor zone. In the long run, this leads to punctate scars becoming visible and to loss of the non-permanent hairs transplanted into the recipient area. Alternatively, it can lead to overharvesting within the safe donor zone, creating visible density gradients in the donor area, often referred to as the windowing effect, or causing diffuse thinning across the donor region in either the short or long term, depending on the degree of overharvesting.
Donor harvesting has a higher risk of exceeding the safe donor as the area of balding expands
Frequently Asked
Questions
+ Who is a good candidate for hair transplantation?
Hair transplantation suitability depends on several factors, including emotional
readiness, the extent of hair loss, and donor hair availability.
Emotional Readiness
Your decision should be personal. If hair loss doesn’t bother you but someone else
suggested the procedure, a transplant is unnecessary. However, if it genuinely affects
you, the next step is assessing both your current and potential future hair loss.
The Severity of Hair Loss: Current vs. Future
A key factor in candidacy is not just how much hair you’ve lost but how much more
you’re likely to lose. Those with current or predicted extensive baldness (Norwood
Hamilton VI or VII) should carefully evaluate their options. Hair transplantation
redistributes existing hair—it doesn’t create new hair—so your donor supply
determines the achievable results.
Ask yourself:
● How much donor hair do I have?
● How much will I need now and in the future?
Ideal Candidates
The best candidates have mild to moderate hair loss (Norwood Hamilton V or less)
and are unlikely to lose much more. In these cases, the ratio of donor hair to balding
areas is favorable, allowing for natural-looking coverage. Ironically, those who need it
least often see the best results.
Poor Candidates
Those with extensive current or predicted hair loss face challenges. If the donor-to-
balding area ratio is low, coverage may be sparse or insufficient. This paradox
means those who need a transplant most may benefit the least.
Predicting Future Hair Loss
Future hair loss is difficult to predict. Age and family history provide some insight, but no
test can guarantee how much more hair will be lost. Younger patients are often eager
for a transplant but face a higher risk of continued hair loss, which can create long-
term cosmetic challenges.
This uncertainty often leads individuals to commit to transplantation without fully
understanding whether they are suitable candidates. Younger patients, in particular,
may seek a solution due to the contrast between their appearance and their peers.
Unfortunately, they are also the most likely to be poor candidates due to early-onset
balding.
While younger patients can undergo hair transplantation, they may be trading short-
term improvements for long-term cosmetic challenges. This doesn’t mean
transplantation is off the table, but it requires a clear understanding of the risks.
Too often, patients assume they will benefit from transplantation without acknowledging
its limitations. A realistic, well-informed approach is essential to achieving satisfying
results and making the right decision.
+ Is it safe?
The procedure is extremely safe. In our practice, there has never been a serious complication, either during or after surgery. It is best regarded as a minor procedure rather than a major operation.
+What hair loss conditions can be treated with hair transplantation?
The most commonly treated conditions are male-pattern and female-pattern hair loss. However, with appropriate precautions and careful patient selection, hair transplantation can also be used to treat other forms of hair loss, including certain scarring alopecias.
+Do I need to be bald before I have a hair transplant?
No, it is entirely possible to add hair to thinning areas of the scalp without damaging existing hair, provided that grafts are placed carefully and aligned with the angle and direction of the native. Our preference is to operate earlier, before individuals become profoundly unhappy with their hair loss and at a time when the procedure can be more easily camouflaged.
+Do I have to be a certain age in order to undergo hair transplantation?
No. Individuals can consider a transplant at any age if they are bothered by their appearance. Younger patients often have a milder degree of thinning, but the emotional impact of hair loss can be particularly significant, making treatment proportionally more important. Although many younger individuals request aggressive, high-density graft placement, they paradoxically require a more conservative long-term surgical plan. Just as there is no minimum age for the procedure, there is also no maximum age limit.
+Are women candidates for hair transplantation?
Yes. A large percentage of women experience hair loss, and many are excellent candidates for hair transplantation. In general, women face fewer long-term aesthetic risks with transplantation, which often makes the procedure more forgiving. However, this reduced downside is balanced by some limitations in potential benefit. Because women more commonly experience diffuse thinning, the donor hair available for redistribution is often less permanent. As a result, transplantation in women tends to “turn back the clock” rather than provide a permanent correction, offering meaningful but typically time-limited improvement.
+Do you guarantee a certain number of grafts?
No. We can provide an estimate of how many grafts we expect to harvest, but surgical variables ultimately determine the final number. Adhering to a precise number risks encouraging surgeons to alter their plan to meet a target rather than respond to the clinical realities on the day of surgery.
+How many grafts are transplanted during surgery?
In a single session, we typically transplant 2000-3000 follicular unit grafts in males and 1500-2000 in females. This number reliably produces a noticeable cosmetic improvement while limiting certain risks. Larger sessions allow treatment of a broader area in one procedure, but may require shaving the scalp to facilitate timely graft placement. It is also important to note that larger sessions carry a marginally higher risk of complications in both the donor and recipient areas.
+How dense are grafts placed?
Grafts are typically transplanted at a density of 30–35 follicular units per square centimeter. This provides meaningful cosmetic improvement while avoiding the use of an excessive number of grafts in a limited area. Mathematically, it is not possible to restore full native density to a thinning scalp without sacrificing the size of the area treated. In other words, there is no such thing as a free lunch. Although older individuals with small, stable areas of thinning may be candidates for higher-density placement, this approach should be avoided in younger patients due to uncertainty about how large their donor and recipient areas may become over time.
+Will I need to shave my head for the procedure?
Dr. Unger offers a no-shave technique. Although operating through longer hair increases the time required to perform the procedure, it makes it easier to follow existing hair patterns and therefore helps produce a more natural result. Equally important, the longer hair provides camouflage, resulting in significantly less visibility during the post-operative period.
Patients who wish to undergo a larger session may need to shave the recipient area to allow timely graft placement. Those undergoing FUE will typically require shaving of the donor are, unless it is for a smaller session.
+Are transplanted grafts visible?
Hairs are implanted in the same way they are removed as individual follicular units, ensuring that the results always look natural. This contrasts with older techniques, in which larger grafts were placed and could appear as unnatural clumps of hair.
+How many operations do I need?
Over a lifetime, most individuals require multiple sessions, although this depends on their goals, the size of the initial area needing treatment, and how their hair loss progresses. We often conceptualize the scalp as comprising three regions: the frontal area, extending from the hairline to a line drawn between the ears; the midscalp, extending from the frontal region to the point where the scalp begins to slope downward; and the vertex, from the midscalp to the rear hair fringe.
Most patients ultimately require treatment of the frontal and midscalp regions at minimum. These are the most important aesthetic zones, as they shape how patients see themselves and how others see them. In particular, restoring the frontal area reframes the face, and this framing effect is often the most impactful part of hair transplantation.
The crown can be transplanted if patients desire and if sufficient donor reserves exist, but it is typically the least important aesthetic region. In many ways, crown transplantation benefits “the view of the neighbour” more than the patient, because individuals rarely see this area themselves.
+Is it safe to travel abroad for a hair transplant?
People can receive either a good or a poor hair transplant, whether the procedure is performed in Turkey, in Canada, or anywhere else. The deciding factor is not the country but the quality of the physician and clinic. The major issues that differentiate clinics are their aesthetic judgment and their long-term planning.
Aesthetically, the biggest pitfalls include constructing hairlines that are too low, too straight, or too coarse. From a planning perspective, common problems include operating on individuals who are poor candidates, planning recipient areas without accounting for future hair loss, depleting the safe donor area, or harvesting outside the true safe donor zone by mistaking the current visible donor fringe for the permanent one.
Additional considerations with international clinics include limited oversight of infection-control standards and reduced transparency regarding physician credentials. Choosing a surgeon who is a member of the ISHRS, which maintains educational standards, clinical practice guidelines, and a code of conduct, provides some assurance of quality.
Perhaps the least significant concern, though often top of mind for patients, is the distance from their clinic in the event of a medical complication. Given that complications are exceedingly rare, this is a minor issue for most individuals.